Case presentation
A 37-year-old woman presented to our OPD complaining of urinary frequency, urgency and incontinence that had been troubling her since two years. The patient complained of pain upon filling of the bladder and the pain diminished with emptying of the bladder. She also reported post-void urgency, increased voiding frequency (more than 10-12 times daily) together with nocturia. She mentioned that she always a feeling of urgency to void and that these symptoms were adversely affecting her posture while walking and sitting as well as her sleep patterns. At times, she also experienced urine incontinence when she rushed to the washroom.
Case history
She had undergone a C-section for the delivery of her second child two years ago, and she began experiencing these symptoms in the aftermath of the operation.
In the past 2 years, she also noticed dull lower abdominal pain occurring infrequently and accompanied with a sensation of weighing down. She sought the help of several doctors in the past and attempted several medications including propiverine, solifenacin and tolterodine. However, the symptoms persisted and that is when she decided to visit our hospital.
Investigations
Physical examination
- The general physical examination revealed that the patient had fever (102ºF) and pallor.
- Per abdominal examination revealed lower abdominal tenderness with abdominal distension, suspected to be either due to gas or ascites.
Laboratory investigations
- Blood tests showed leukocytosis (16,500 WBCs/mm3) with greater proportion of polymorphic cells (83%). The patient was found to be anemic, with Hemoglobin at 7.9 gm%.
- Urinalysis demonstrated the presence of few pus cells and a few red blood cells (RBCs 2-5 in HPF).
Voiding chart, urodynamics and cystometry
The frequency-volume chart revealed that the patient had to void a volume of 70-150 mL every 30-60 minutes, thereby indicating subnormal functional bladder capacity.
An urodynamic study was advised, which revealed phasic detrusor over activity.
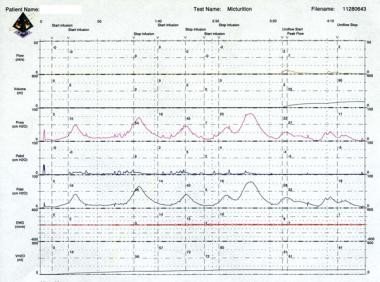
Cystometry was subsequently planned. Presence of multiple uninhibited detrusor contractions (phasic contractions) generating 40- to 75-cm water pressure during the filling could be noted, as shown in Figure 1, accompanied by urinary incontinence. She also had small bladder capacity (81 mL), indicating poor bladder compliance.
Cystoscopy
Cystoscopy showed diffuse glomerulations and marked terminal hematuria, as depicted in Figure 2.
Diagnosis
Based on the above investigations and correlating the same with the patient’s clinical presentation, a diagnosis of Painful Bladder Syndrome (PBS)/ Interstitial Cystitis (IC) was made.
Treatment and Follow-up
The patient was then started on oral pentosan polysulphate 100 mg TID along with bladder training. The patient reported significant improvement in her symptoms at the end of first month and was continued on the same therapy. At the last follow-up at 3 months, the patient had a remarkable recovery and persistent relief of her symptoms.
Discussion
Interstitial cystitis/ painful bladder syndrome (IC/ PBS) is a chronic, painful and disabling condition of the urinary bladder and its prominent features include suprapubic pain and urinary symptoms such as urgency, nocturia and urinary frequency.1-3 The principal characteristic of this condition is pain other symptoms are known to exacerbate the condition. The name painful bladder syndrome (PBS)/ bladder pain syndrome (BPS) was coined by the European Society for the Study of IC/BPS (ESSIC), which established that PBS/ BPS should be diagnosed by “the presence of chronic pelvic pain lasting more than 6 months, pressure/discomfort perceived to be related to the urinary bladder, and one or more urinary symptoms such as urinary urgency or frequency.”2,4 The American Urological Association (AUA) ascribed IC/BPS to be “an unpleasant sensation (pain, pressure, or discomfort) perceived to be related to the urinary bladder, and associated with lower urinary tract symptoms of more than six weeks duration in the absence of infection or other identifiable cause.”2 Other globally recognized bodies, such as the National Institute of Health-National Institutes of Diabetes, Digestive, and Kidney Disease (NIDDK) and the International Incontinence Society have also proposed varying definitions for IC/ PBS. Females are at a greater propensity to develop this condition.5
There exist several ambiguities as regards the etiology, pathophysiology and diagnostic modalities employed in PBS.6 However, a multidisciplinary approach needs to be adopted in the evaluation and management of interstitial cystitis/bladder pain syndrome.7
In the present case scenario, the patient presented with complaints of urinary frequency, urgency and incontinence following a C-section 2 years ago and that the pain was intense upon filling of the bladder and bettered upon voiding. While she had sought several treatment modalities prior to approaching us at our center, they seemed to be futile as her symptoms persisted.
Following preliminary physical examination and laboratory investigations, she was advised to undergo urodynamic studies and cystometry and to maintain a voiding chart.
The frequency-volume voiding chart helps understand voiding habits over a period of 24 hours.8 Earlier, a three-day chart was preferably used; however, it has been demonstrated that a 24-hour chart could replace the same and effectively serve the purpose as well.9 Urodynamic studies were heretofore not recommended to be used in routine practice. Yet, strong evidences correlate the utility of urodynamics with other parameters such as severity of glomerulations and maximal bladder capacity. Moreover, it can be effectively used to differentiate IC/PBS amongst women with increased distension of the bladder.10 Cystometry is aimed at identifying patient symptoms and correlating them to synchronous urodynamic events. The procedure enables detailed understanding of bladder sensations, bladder compliance, detrusor overactivity (DO), and maximum cystometric capacity.11
A cystoscopy subsequently carried out demonstrated diffuse glomerulations and marked terminal hematuria. Cystoscopy is the “gold standard” for the diagnosis of IC in clinical practice.12 It helps to objectively classify patients that are often clinically indistinguishable and there are several methods by which cystoscopy is carried out, in accordance with various guidelines.6 However, the AUA Guidelines advocate the use of cystoscopy together with urodynamics only in the event of complex presentations.6,13
The patient was managed using pentosan polysulphate 100 mg TID per oral together with appropriate bladder training. The patient showed complete recovery from symptoms by the end of three months of initiation of treatment.
The recently published Canadian Urological Association Guidelines ascribe a prominent place to pentosan polysulphate in the management of IC/ PBS.14 In fact, pentosan polysulphate is a polysulphated xylan and the only FDA-approved oral medication to treat IC/ PBS.15
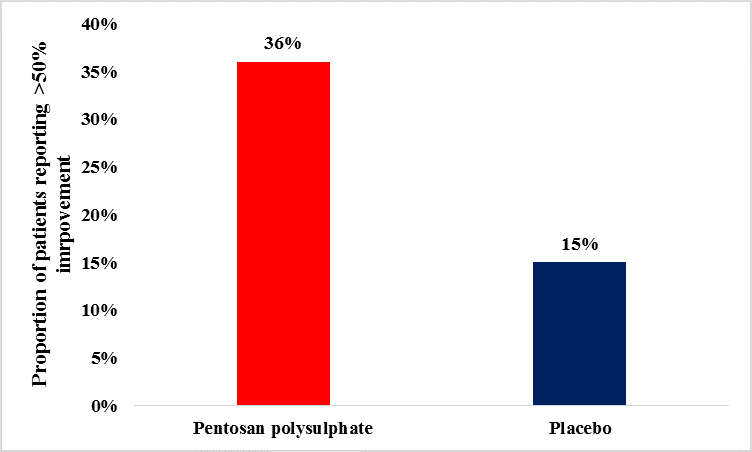
Studies have demonstrated greater efficacy outcomes among pentosan polysulphate-treated vs. placebo-treated, as documented by patients reporting an improvement >50%.16 These results have been depicted in Figure 4.
Putting together the available literature in the field, it can be conclusively inferred that treatment with pentosan polysulfate was appropriate in the given circumstances, as seen from prompt and complete resolution of symptoms.